About Me
Hello everyone, my name is Henrik Maltzman. I am foremost a physician at Karolinska University Hospital in Sweden, with special focus on removing early cancer and precancerous lesions in the gastrointestinal tract using endoscopy. With techniques such as ESD (Endoscopic Submucosal Dissection) we can locally resect tumors that previously would have required more invasive surgical procedures. I am also a PhD student as of last year, honestly a bit late blooming since I am already 40 years old. Because of my role also as a clinician I’m involved in the Endeavor team in two different ways – as part of the research team and also in the clinical management of patients.
Barrett’s Esophagus & ENDEAVOR
Barrett’s esophagus is a condition in the lower esophagus affecting up to 5% of the general population, caused by acid reflux. As such, it can barely be called a disease but rather a risk factor for esophageal cancer. The hallmark for Barrett’s is a change in the type of cells in the esophageal mucosa from the ordinary squamous epithelium (not much unlike the cells in the mouth or throat) to cells resembling the normal small intestine. This cell change is called intestinal metaplasia in our medical language, and the presence of such cells is the basis of the diagnosis of Barrett’s.
It is important to emphasize that most patients with Barrett’s have a low overall risk of developing esophageal cancer or precancerous lesions (see Figure 1 for an example of Barrett’s esophagus with an early cancer).
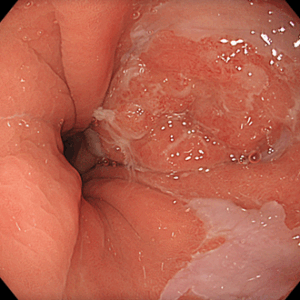
Figure 1. Barrett’s esophagus with early cancer at 2 o’clock position.
As the numbers of patients are vast, this poses a clinical dilemma for us as doctors – which patients should we monitor closer and which could we see more seldom? The same problem applies to patients that have an early cancer removed by us. The absolute majority of these patients will have an excellent prognosis and a low risk of new events. However about 10 % can have a more aggressive disease and either develop new tumors in the remaining Barrett’s, or even metastasis. How do we know which patients to prioritize and follow more closely?
The latter question is currently being addressed in our Endeavor trial, and I am proud to be part of the research team. In the project, we are looking at specific genetic abnormalities that could indicate a worse outcome after endoscopic removal of a Barrett’s tumor. In my clinical practice, I see patients like this every week. Apart from the obvious concerns of being diagnosed with cancer, these patients also face the burden of frequent follow-up endoscopies, radiological exams, and other interventions. If the Endeavor study could find ways of individualizing this follow-up based on the patient’s genetic risk, this could be of great importance for many of my patients that are often elderly and suffer from other medical conditions.
My other research
In my own research, I am studying various themes in upper gastrointestinal cancer from an endoscopic perspective. The main part of my doctoral thesis is outside of the Endeavor umbrella. It encompasses the whole spectrum of what we do in endoscopy – from detection of early dysplastic changes in conditions such as Barrett’s all the way to treating advanced gastric cancer in patients that are too frail to withstand normal surgery. By combining clinical research and my work as a clinician, I hope to make a meaningful impact on both patient care and the broader medical field. People like me will probably never be top-tier academic researchers, but our strength is that we know very well what is relevant to actual patients and in real life problems in the clinical realm. Together with the preclinical and lab oriented scientists, we can forge an alliance to withstand the challenges of treating Barrett’s and other conditions in the upper gastrointestinal tract.
Henrik Maltzman

