About Me
Hello everyone, my name is Nastaran Riahi. I am a PhD Candidate in Oncology at the University of Antwerp and a Clinical Researcher at Universal Diagnostics (UDX).
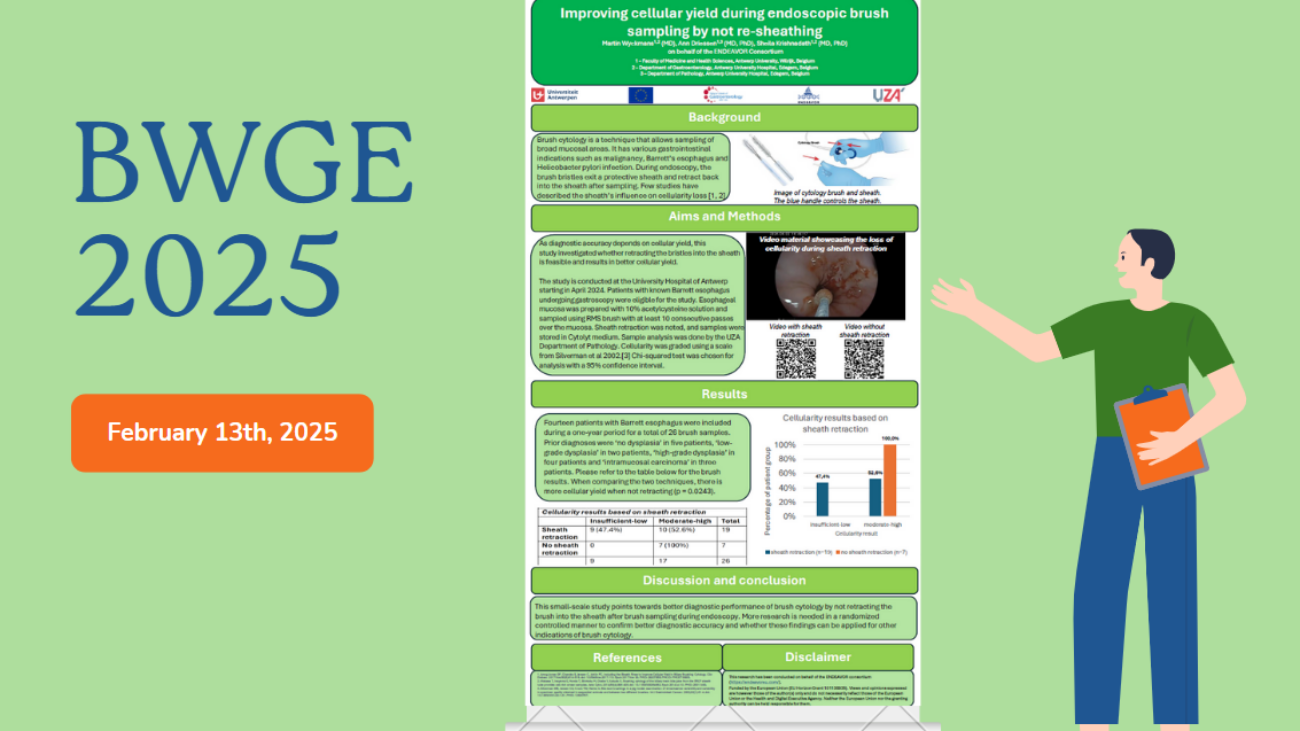
When I joined UDX five years ago as a cancer researcher, I was captivated by a simple, powerful idea: could a routine blood test help us detect cancer and its precursors early enough to change someone’s story? That question led me to pursue my PhD at the University of Antwerp within the ENDEAVOR project, under the supervision of Prof. Dr. Krishnadath, who leads this European initiative. ENDEAVOR is a five-year, EU-funded collaboration bringing together 15 academic partners, two general hospitals, and UDX as an industry partner. Our shared goal is to translate that “simple blood test” idea into practical tools for people living with Barrett’s esophagus (BE).
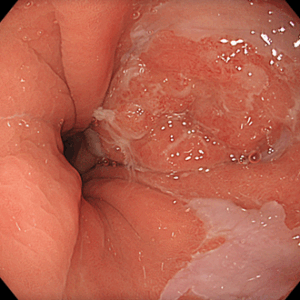
Why Barrett’s Esophagus and Why Now?
Esophageal cancer is one of the deadliest cancers worldwide because it’s often found late and behaves aggressively. Esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC) are the two most common histological subtypes of EC. Over four decades, the frequencies of EAC and BE, the known precursor lesion for EAC, have sharply increased in North America and Europe. Despite early detection and endoscopic therapy, the patient’s clinical course remains difficult to predict. That uncertainty means many patients undergo frequent, invasive endoscopies. Since no other modality of surveillance is currently available. We can do better.
ENDEAVOR’s goals
ENDEAVOR aims to build smarter risk-stratification for BE: helping clinicians see earlier and more precisely, who is likely to progress and who will respond well to treatment. The vision is personalized prevention, directing the right treatment at the right time and tailoring follow-up so patients avoid unnecessarily invasive procedures while remaining cancer-free.
My Project in a Nutshell
My PhD focuses on whether a multi-omics approach combining DNA methylation signals in blood with genetic mutations identified in tissue can predict how BE patients respond to endoscopic therapy and who is at the highest risk for EAC. In practical terms, I analyze cell-free DNA (cfDNA) from blood samples taken before and after endoscopy treatment, using targeted methylation sequencing developed at UDX. Then, with the ENDEAVOR collaborator, I integrate those data with matched tissue mutation profiles. The hope is to create a robust set of biomarkers that distinguishes responders from non-responders to treatment and guides clinical decisions.
Why Methylation?
Among many potential biomarkers, aberrant DNA methylation has emerged as one of the most promising for monitoring BE and detecting EAC early. By reading methylation changes in cfDNA, we may capture a real-time picture of tumor biology from a simple blood draw. Pairing that with mutation data can reveal how genetics and epigenetics work together during disease progression and how they respond to treatment.
How We’re Doing It
- 1. Who we study: In the pilot study, approximately 50 patients with high-grade dysplasia (HGD)/ early EAC are at the highest risk for progression.
- 2. When we sample: Two time points, before treatment and after completion (e.g., after endoscopic mucosal resection (EMR)and/ or endoscopic submucosal dissection (ESD) and before radiofrequency ablation (RFA)), to see how molecular signals shift with therapy.
- 3. What we measure:
- A) At UDX, we perform hybrid-capture targeted methylation sequencing on cfDNA and process results with proprietary signal-processing and machine-learning tools for precise, fragment-level scoring.
- B) Partner performs exome sequencing on matched tissue within ENDEAVOR to map somatic mutations.
- C) We then integrate both layers to build prediction models for treatment response and risk.

The Role of UDX
UDX is a Spanish diagnostics company building blood tests that can “read” cancer and precancer signals at their earliest stages. Our platform, already used in colorectal cancer detection programs, brings three things to ENDEAVOR:
- Targeted methylation assay development and sequencing,
- Advanced signal processing at the read/fragment level, and
- Machine-learning pipelines for risk stratification.
What Success Looks Like
If we get this right, patients could have access to:
- 1. A minimally invasive blood test that helps forecast who will respond to endoscopic therapy and who may need closer monitoring or alternative strategies.
- 2. Sharper risk-stratification to personalize surveillance intervals, reducing unnecessary procedures for many, while focusing attention where it matters most.
- 3. A path to earlier intervention, when treatments can be most effective and lives most changed.
A Personal Note
As a clinical researcher, I’m motivated by the patients behind every tube, dataset, and model. ENDEAVOR lets me work at the intersection of academia and industry, combining the methodological discipline of a university PhD with the translational power of UDX’s technology. It’s a privilege to work alongside clinicians, bioinformaticians, and scientists across Europe who share a simple aim: to make care predictive, patient-centered, and more precise for people with Barrett’s esophagus.
Nastaran Riahi